DVT Claims More Lives Than Breast Cancer, HIV, and Motor Vehicle Crashes Combined!
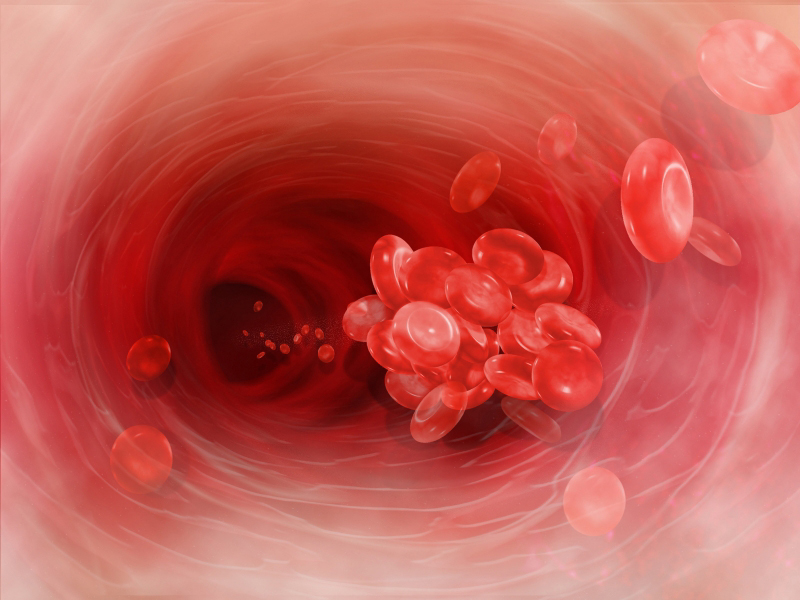
| Red blood cells clumped together form a blood clot (thrombus) that can block blood flow in the body's deep veins, and cause DVT. |
Deep vein thrombosis (DVT) can be a dangerous medical condition caused by the creation of a blood clot (thrombus) in a deep vein of the leg or lower pelvis. Pulmonary embolism (PE) happens when a DVT starts to move through your body and gets stuck in the lungs. This can be life threatening or deadly all of a sudden.
The term venous thromboembolism (VTE), which means a blood clot that starts in a vein, is used to describe both conditions.
DVT can affect people of all ages and backgrounds. Personal risk factors for DVT may change throughout your lifetime depending on your health and events that may change your risk.
It is important to understand your personal risk factors, take steps to prevent DVT, and recognize signs and symptoms if they happen. If you think you may have a DVT, it is very important to seek medical care right away.
Be involved in your care — take steps to prevent DVT blood clots!
Facts
The CDC estimates as many as 900,000 people could be affected each year in the United States by a DVT or a PE. It is also suggested that 60,000-100,000 Americans die of a DVT or a PE. This is more deaths than seen from breast cancer, HIV, and motor vehicle crashes combined.
DVT/PE are often underdiagnosed. In fact, 10% to 30% of people will die within one month of diagnosis. Sudden death is the first symptom in about 25% of people who have a PE. It is important to know about DVT/PE because it can happen to anybody at any age, but more in the elderly population.
Half of the people who have ever had a DVT will have long-term complications, such as swelling, pain, discoloration, and scaling in the affected limb. A third of the people with DVT/PE will have a recurrence within 10 years.
The good news: DVT is preventable and treatable if discovered early.
Risks
Being hospitalized, obesity, varicose veins, or sitting too long in car rides or plane rides can cause your leg blood flow to slow down and gather in one spot. This is an easy way for a clot to form.
Cancer, pregnancy, taking birth control, hormone replacements and/or smoking make the blood clot easier by making the blood sticky.
Surgery or a big trauma can cause a DVT because the blood vessel is damaged and tries to fix itself with a blood patch.
Symptoms to Look For
PE symptoms include:
- Abnormal rapid breathing
- Chest pain when taking a deep breath
- Fainting
- Rapid heart rate
- Shortness of breath
- Bloody cough
DVT symptoms include:
- Pain
- Tenderness
- Swelling
- Warmth
- Redness
If you have any of the symptoms of a DVT, it is important to seek urgent care from your doctor. To see if you have a DVT, they will do an ultrasound on your leg(s). This is a wand that is moved along your leg(s) to see if you have a DVT.
If you experience any of the symptoms of a pulmonary embolism,
it is an emergency and you should seek medical attention immediately!
To test for a PE, you will need a CAT scan of your chest. A special dye will be put in your vein through an intravenous line (a small catheter in your vein) to take a better picture.
Prevention
Even if you have risk factors, there are a number of things you can do to decrease your risk. Exercise regularly and maintain a healthy weight. Don't smoke!
If you travel for longer than six (6) hours or are sitting for long periods of time, you should exercise your legs frequently, get up and walk around every two to three hours. Wearing loose-fitting clothing and keeping well hydrated (but staying away from caffeine and alcohol) also can help reduce your risk.
Before and during any hospitalization, talk to your healthcare provider about your risk of blood clots and what can be done to help prevent them. If you have to remain in bed, move around as much as possible and get up when your practitioner says it is okay.
During your hospital stay, you may be given a small dose of an anticoagulant (blood thinner) to help prevent DVT. If a mechanical device such as compression sleeves and pump are ordered, it is important to keep it on at all times except when walking.
| Talk to your doctor about your level of risk! While we sincerely hope you or someone you love never experiences a DVT, it is important to know you have access to advanced treatment and expertise here at Stony Brook University Hospital. Our specially-trained DVT team is an award-winning team that has reduced the amount of hospital-acquired DVTs. You can also receive outpatient care at our Centereach and Commack locations that specialize in veins for immediate and long-term care. The team is led by Antonios P. Gasparis, MD, professor of surgery and member of our Vascular and Endovascular Surgery Division. |

