Testimonials of Patients Treated at Stony Brook Medicine
Stony Brook University Hospital is the only hospital on Long Island to provide cytoreductive surgery (CRS) and HIPEC — heated intra-peritoneal chemotherapy — for the treatment of advanced abdominal cancers.
The CRS-HIPEC procedure is an aggressive combination of surgery and chemotherapy to eradicate abdominal tumors. The goal of CRS and HIPEC is to perform radical surgery to remove all disease, but also to enable return to regular daily activities.
In select patients, HIPEC may increase survival time significantly. It offers patients hope when hope is needed most. It's a special form of surgery and intraoperative chemotherapy first performed in 1979, and further developed since then.
Here are answers to frequently asked questions about CRS and HIPEC provided by our surgical oncologists at Stony Brook Medicine.
Q: What is CRS?
A: CRS is short for cytoreductive surgery. It is simply the removal of all sites of cancer within the abdominal cavity. However, the operation itself is not simple and should only be performed by experts with many years of experience.
Q: How is CRS different from regular surgery for abdominal cancer?
A: CRS is very different from standard operations for abdominal cancer. In most instances, patients with peritoneal carcinomatosis (disease that has spread in the peritoneal cavity) are not offered operations since these patients are considered to have unresectable disease, that is, cancer that cannot be removed with surgery.
However, CRS has been shown to be effective in carefully selected patients with peritoneal carcinomatosis. The goal of our surgical oncologist at Stony Brook is to remove all visible cancer in the abdominal cavity. Since most surgeons have limited surgical experience with peritoneal carcinomatosis, it is very important to find surgeons with years of experience in this setting.
Q: What is HIPEC?
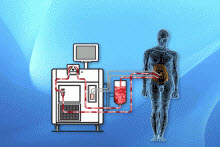
A: HIPEC is short for hyperthermic (heated) intra-peritoneal chemotherapy. It is simply the administration of heated chemotherapy solution into the abdominal cavity of patients with peritoneal carcinomatosis.
The heated chemotherapy is delivered into patients while they are in the operating room during the CRS procedure. The heated chemotherapy can be delivered using either the open or closed techniques, when the skin is either sewn closed or left open during the chemotherapy procedure.
Q: How does HIPEC work?
A: CRS and HIPEC work together to eradicate and kill all cancer cells. With CRS, all gross and visible cancer cells are removed. With HIPEC, the remaining microscopic cancer cells are treated. The heat and chemotherapy work in combination to eradicate and kill cancer cells.
Patients should seek surgeons with established track records of performing these complex operations.
Q: What types of cancer is HIPEC used to treat?
A: Our team has close to two decades of experience using HIPEC to treat patients with gastric cancer, colorectal cancer, appendiceal cancer, intra-abdominal sarcoma, and gynecologic cancers.
Q: Why is HIPEC preferred over traditional chemotherapy?
A: Traditional chemotherapy is given through the intravenous route to reach the cancer targets. Unfortunately, the disease in peritoneal carcinomatosis often has poor or limited blood supply; therefore, it is more difficult for intravenous chemotherapy to reach these tumors to kill them. HIPEC allows direct contact between the chemotherapy drugs and microscopic cells that remain in the peritoneal cavity.
Q: Is HIPEC experimental? Does health insurance cover it?
A: HIPEC is not experimental and studies have verified that it is an effective and safe procedure in experienced medical centers. It is a procedure that is covered by insurance, and our team has experience with helping obtain insurance coverage for both in-state and out-of-state patients.
Q: How safe is the CRS-HIPEC procedure?
A: There are numerous reports showing that this procedure may be dangerous and risky. With our years of experience, we have performed this procedure safely with zero mortality.
Q: What training must a surgeon have for performing this procedure?
A: There is no formal curriculum for training in CRS and HIPEC, so patients should seek surgeons with established track records of performing these complex operations.
Q: Who is a candidate for HIPEC?
A: It is clear that many physicians, including surgeons, do not know or understand the CRS and HIPEC procedure. In many instances we see patients who were told by their physicians that they had no options. Any patient with cancer that remains confined to the peritoneal cavity may be a potential candidate for CRS and HIPEC.
We provide an online consultation service for patients who seek a second opinion on the management of their cancers. We are available to review radiographic imaging and discuss treatment options. Interested physicians and patients should call our office at 631-444-8086.
Q: How long does it take to recuperate from the CRS-HIPEC procedure?
A: Most of our patients have a hospital stay of approximately 7-10 days. In some cases, the hospitalization could be shorter or possibly longer. For all of our patients, our expectation is that they will return home after surgery being able to complete their normal daily home activities.
Q: What is the advantage of having the CRS-HIPEC procedure done at Stony Brook Medicine?
A: We have a multidisciplinary team (surgery, radiology, pathology, medical oncology, social work) that is highly experienced in providing CRS and HIPEC for patients from New York State and beyond.
For more information about CRS and HIPEC, visit the Appendix Cancer Connection and PMP Pals. For appointments to have a consultation with our CRS-HIPEC specialist, please call 631-444-8086.